Stress in early life – the impact on mental illness
25 April 2017
You’re under threat.
Your brain reacts instantly. Like a runner at the start line of a race, it springs into action as if the threat was a gunshot.
The hypothalamus gets the ball rolling, sending chemicals to the pituitary gland. The pituitary spills out hormones to a second gland, called the adrenal gland. Adrenaline and glucocorticoids flood out of the adrenals, rushing around your entire body.
Your heartbeat increases so you can hear the blood thumping in your ears. Your muscles tense, your blood pressure goes sky-high. You breathe harder and deeper. Sugar, known as glucose, is released from your liver; ready for you to react.
As you stand, rigid and poised to run or fight, the threat vanishes. Maybe the car swerves around you; maybe you find the light switch in a dark unknown room. Your brain tells all these systems that it is time to go back to normal. Their job is done. Your muscles relax and you take a deep sigh of relief.
This system is called the hypothalamic-pituitary-adrenal axis (HPA axis) and it is highly important because it has evolved with the sole purpose of increasing your probability of survival.
However, what happens when this system doesn’t know how or when to switch off?
Stress response going awry
The ‘start’ and ‘stop’ nature of this stress response is the key to its success and the correct working of the body and brain. Like every tightly controlled system, if one part goes wrong, a lot more goes wrong, too.
Think of it like an electrical circuit controlled by a switch; it only works effectively if all the components work together and the switch is ‘on’. If any one of the wire connections or electric components malfunctions, it can have a detrimental effect on the circuit. Therefore, it may not be too much of a surprise to learn that this intricate axis is associated with many disorders. Sadly, it is particularly implicated in complex illnesses that we struggle to manage, let alone cure, such as schizophrenia.
The chemicals that most anti-depressants and anti-psychotics target – serotonin, dopamine and noradrenaline – all have a direct impact on the HPA axis. The fact that this system can be hit by all the big players in mental illness suggests that this may be a converging point of damage that leads to the onset of schizophrenia. Over recent years, research has started to unravel just how stress can harm the brain, and how this may manifest in the symptoms of schizophrenia.

Trauma in childhood
One of the most consistent factors that increases risk for psychiatric disease is early life stress. Sadly, children who are subject to severe abuse, bullying or neglect are much more likely than their well-cared for peers to go on to develop mental illness as adults. These children, under constant stress, have hyperactive HPA axis’s, releasing chemicals with terrifying regularity and at far too high levels. The system is always stuck on ‘go’, with the off switch missing from the circuit. This can lead to alterations in the normal homeostasis of the body and have a large impact on the brain.
Children’s brains are much more plastic than adults; they are constantly growing and developing. Hitting them with a constant barrage of stress and its associated chemicals can have damaging and irreversible effects that can persist throughout adulthood.
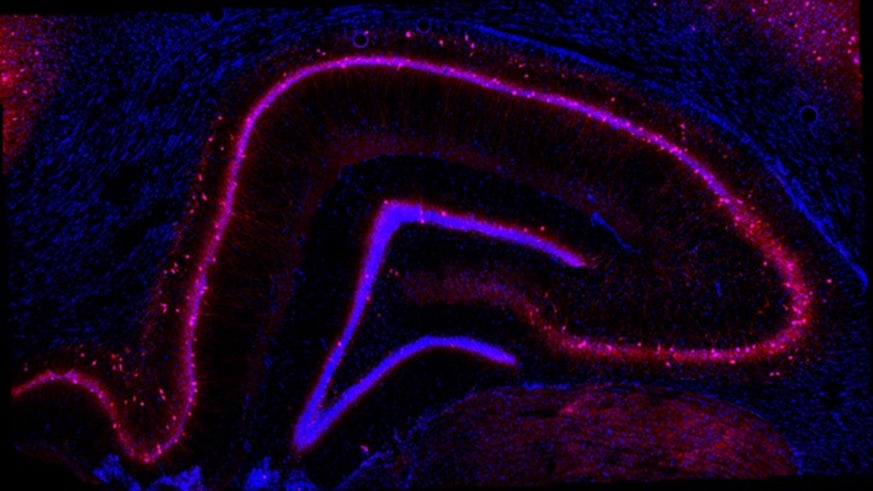
One of the main regions of the brain that is affected by stress is the hippocampus– a structure vital for learning, memory and neurogenesis (where new neurons are made). The cortisol hormone has been shown to physically shrink the hippocampus and cause widespread neuron loss. This in turn can affect not only cognitive processes such as learning, but also has an impact on the HPA axis itself – creating a vicious cycle of stress-induced damage.
Early life stress and gene expression
Each of us has an individual collection of genes that we inherit from our parents. We know that our risk of psychiatric disorders, particularly schizophrenia, is largely based on our genetic material. However, environment can have a profound and lasting effect on the expression of our genes.
My research addresses how early life stress and the various mechanisms it offsets can alter genes that we know are associated with risk of psychiatric disorder.
At the BNA Conference in Birmingham, I presented a research poster that showed how an animal model of early life stress revealed a significant decrease in hippocampal gene expression of Cacna1c, a gene that allows calcium – a molecule essential for many molecular processes – in and out of cells.
Many people with psychiatric disorders such as schizophrenia have alterations in this gene. Decreases in the gene can lead to altered neurogenesis – the process of making new neurones in the hippocampus and altered fear behaviour.
This suggests that stress in early life can lead to lasting effects on gene expression, potentially through epigenetics, that can impact on biological mechanisms and behaviour. This may offer an insight into how psychiatric symptoms can manifest themselves in adulthood.
Looking to the future
If we can tie together how genes and environment may work together to contribute to the development of psychiatric disorder, it is exciting to think we will be one step closer to understanding these complex conditions. One major problem with treating these disorders is there is no real understanding of how they work. We need to fully understand the underlying mechanisms that cause mental illnesses, and how they may be caused by more than one factor, potentially acting together, in order to create novel and more effective treatments.
