The immune system and the brain: complement or casualty?
18 April 2017
For a long time it has been assumed that the sole purpose of the immune system is to defend the body against infection. However, research is now showing that your immune system is doing much more than this...
In fact, it is doing some extremely clever multitasking. These non-immune duties are important for the healthy development of your brain and consequently your mental health. If they go awry, they may cause mental disorder.
Pruning for an optimally connected brain
The complement system is an ancient branch of immunity, which serves as a ‘first defence’. Upon encountering bacteria or a virus-infected cell, whilst other immune system regiments are carefully selecting their armoury, complement swiftly launches an attack by recruiting phagocytes – cells that literally engulf pathogens – with fatal consequences.
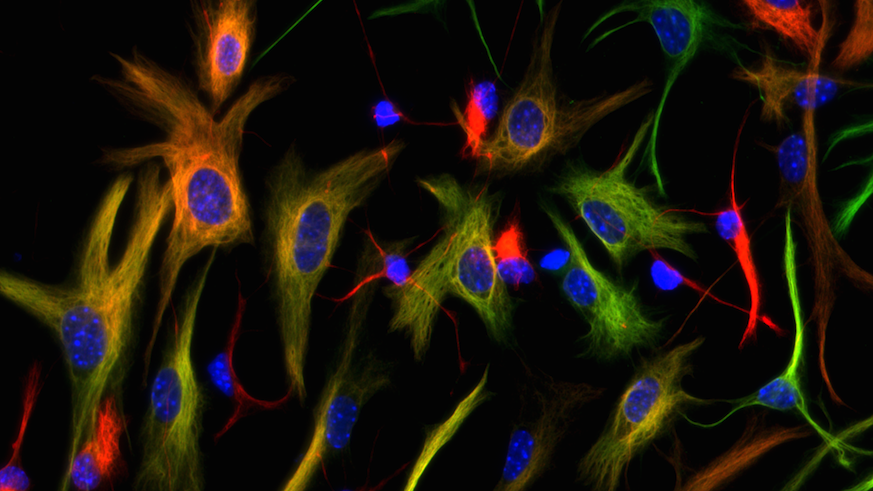
Shocking it may seem, but throughout childhood and early adulthood, evidence from animal models suggests that complement directs this same mechanism upon your own brain cells. When you are born, each brain cell – or neuron – has many more connections than it needs. In order to communicate more effectively, these connections are gradually reduced or ‘pruned’, until eventually only the necessary, strong connections remain in place for adulthood. This process is known as synaptic pruning.
It is now known that complement is involved in this process. It ‘tags’ connections that are not routinely used, and attracts the brain’s phagocytes, known as ‘microglia’ (a type of cell found throughout the brain and spinal cord), to literally gobble up the unnecessary connections. While it does seem somewhat cannibalistic, this process is thought to lead to an optimally connected brain.
The overzealous gardener
However, we are all guilty of the old adage, ‘eyes bigger than our bellies’ (especially at a buffet…) and complement is no exception. In some instances, it may gluttonously gorge on neuronal connections, with dire consequences.
In the brains of patients with schizophrenia, a severe mental disorder characterised by delusions, hallucinations, and memory impairments, scientists now think that complement has acted akin to an overzealous gardener.
Indeed, patients and mouse models of schizophrenia show a reduced number of connections between their neurons, amongst other abnormalities. Not coincidentally, mutations in the DNA instructions for complement have been found more often in patients with schizophrenia when compared to the healthy population. It is thought that these mutations cause complement to become overactive.
What’s more, microglia have also been shown to be hyperactive in the brains of people with schizophrenia. Together, this combination may lead to excessive pruning during brain development. Scientists have speculated that the resulting abnormal brain connectivity may give rise to the debilitating symptoms of the disorder during adulthood.
This process of synaptic pruning is thought to diminish as your brain matures in your 20s. However, complement has its ‘fingers’ in many a pie, and continues to play an important role beyond this period of life.
Whilst most of your brain development is now complete, there is a particular area in which there is ongoing renewal throughout your entire life. This area, known as the hippocampus, is special because within it resides a pool of stem cells. These are primitive cells that give birth to new neurons throughout adulthood, a process known as neurogenesis. These new neurons are critical for your ability to make new memories and also for regulating your mood and emotions.
Research into brain disorders
During my PhD, I have found that complement regulates the number of new neurons born in the hippocampus, and can also change their structure, ultimately affecting their connectivity. In disorders such as schizophrenia, epilepsy and depression, which are known to have heightened complement activity, abnormal neurogenesis may play a role in patients’ memory and mood problems, and is therefore a valuable target for therapeutic intervention.
At this year’s BNA Conference in Birmingham, my research poster presentation shows how complement may determine how you would feel if you were to teeter on the edge of a very high cliff. Mice lacking a receptor for an important complement protein show heightened anxious behaviour when placed in a harmless but fear-evoking situation, though this appears to be independent of the effect of complement on neurogenesis.
The impact of complement doesn’t stop there, either. Scientists now think that complement may regain its feisty appetite for neuronal connections during ageing, where excessive pruning of connections may contribute to the loss of brain cells seen in neurodegenerative conditions such as Alzheimer’s disease.
Controlling synaptic pruning
There is a desperate need for new therapeutics in psychiatry. As a Wellcome Trust Integrative Neuroscience PhD researcher and a Waterloo Foundation Early Career Research Fellow, my aim is to further understand how the immune system interacts with development and the adult brain to produce these devastating illnesses, and how we can prevent it.
Many current drug treatments target the symptoms of psychiatric disorders, without addressing underlying causes. In contrast to physical illnesses, this is largely due to our ignorance of the actual mechanisms that give rise to mental health diseases. It is hoped that this vital area of research will further our understanding of the causes of schizophrenia and related diseases, in an attempt to generate novel therapeutics which will improve the way in which psychiatric disorders are diagnosed, treated and eventually, prevented.
