Investigating a placental origin for pregnancy and postpartum mood disorders
1 March 2015
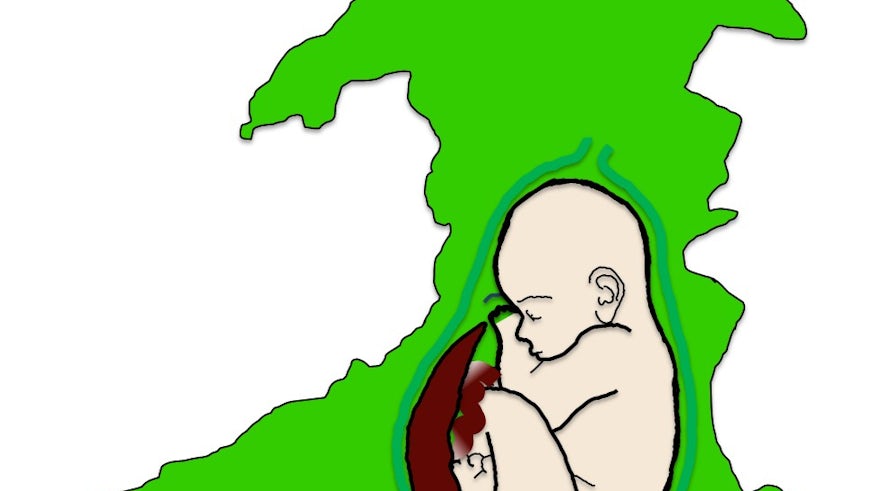
Providing a biological explanation for the relationship between pregnancy and maternal mood disorders represents one of the greatest challenges of perinatal medicine. Psychiatric illness is the leading cause of maternal death in the UK and one in five women will develop some form of mental health issue during pregnancy and the months after childbirth. While in most cases normal mood is restored, chronic depression and anxiety during pregnancy is associated with low birth weight while both pre and postnatal mood disorders are independently associated with poorer mental health outcomes for children. A key change that occurs during pregnancy is exposure to placental hormones. The placenta is a powerful endocrine organ pumping out vast quantities of hormones acting on the mother to induce changes in maternal physiology required to ensure a safe and successful pregnancy. In addition to securing nutrient transport to the fetus, these changes include the induction of maternal behaviour. Work from Dr Rosalind John’s group at the School of Biosciences provided the first suggestion that imprinted genes, which are regulated by epigenetic marks, influence placental signaling and thus may influence birth weight and maternal behaviour.
This MRC-funded project, led by Dr John, will bring together the expertise of Professor Ian Jones (perinatal psychiatrist; School of Medicine), Dr Anthony Isles (behavioural neuroscientist, School of Medicine) and Mr Richard Penketh (consultant obstetrician; University Hospital of Wales) to explore the hypothesis that the epigenetic misprogramming of placental signals contributes to maternal mood disorders in human pregnancies.
This work will uniquely combine the use of preclinical animal models and human samples to examine the relevance of gene changes in the placenta to pregnancy and postpartum mood disorders. While we are not able to model all aspect of human disease in experimental models, particularly with respect to complex cognitive behaviours, we can determine causal relationships to provide greater biological insight into the origins of abnormal maternal mood. Our work will impact clinicians managing pregnant women and also our perinatal psychiatrist colleagues by providing a new understanding of pathologies underlying to maternal mood disorders. Moreover, it is possible that our work will lead to the development of new diagnostic and predictive tools based on simple biomarkers to support the identification and management of at risk women and their children.